Introduction
Cardiovascular diseases (CVDs) remain the leading cause of mortality worldwide, posing significant challenges to public health systems globally. These diseases encompass a wide array of heart and blood vessel disorders, which can lead to fatal events such as heart attacks and strokes. Our goal is to provide an in-depth, detailed exploration of CVDs, their risk factors, symptoms, and preventive measures, as well as strategies for managing and reducing their burden.
What Are Cardiovascular Infections?
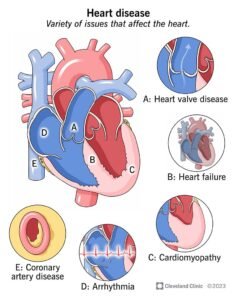
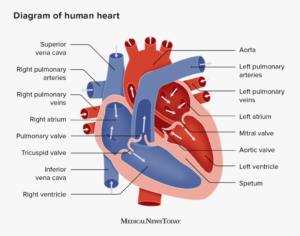
Cardiovascular illnesses are a gathering of problems influencing the heart and veins.. They include:
- Coronary Heart Disease (CHD): A condition where the blood vessels supplying the heart muscle become narrowed or blocked, leading to chest pain (angina) and heart attacks.
- Cerebrovascular Disease: Disorders of the blood vessels supplying the brain, potentially resulting in strokes.
- Peripheral Arterial Disease: Affects blood vessels supplying the arms and legs, leading to pain and mobility issues.
- Rheumatic Heart Disease: Damage to the heart muscle and valves due to rheumatic fever, which is triggered by streptococcal bacteria.
- Congenital Heart Disease: Birth defects affecting the structure and function of the heart.
- Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE): Blood clots in the leg veins that can dislodge and travel to the heart and lungs.
Acute Events: Heart Attacks and Strokes
Heart attacks and strokes are often the first indication of underlying cardiovascular diseases. These acute events primarily result from blockages in the blood vessels that hinder blood flow to the heart or brain. The blockage is commonly caused by the accumulation of fatty deposits on the inner walls of the blood vessels.
heart failure symptoms
heart disease symptoms
congenital heart disease
heart problems symptoms
heart problems
symptoms of heart blockage in females
cardiovascular
ischemic heart disease
cardiovascular disease symptoms
Symptoms of Heart Attacks
- Chest pain or discomfort
- Pain or discomfort in the arms, left shoulder, elbows, jaw, or back
- Difficulty breathing or shortness of breath
- Nausea or vomiting
- Light-headedness or faintness
- Cold sweat and pallor
Symptoms of Strokes
- Sudden weakness or numbness of the face, arm, or leg, especially on one side of the body
- Sudden confusion, difficulty speaking, or understanding speech
- Sudden difficulty seeing with one or both eyes
- Sudden difficulty walking, dizziness, or loss of balance or coordination
- Severe headache with no known cause
- Fainting or unconsciousness
Risk Factors for Cardiovascular Diseases
Behavioral Risk Factors
The major behavioral risk factors for CVDs include:
- Unhealthy Diet: High in saturated fats, trans fats, salt, and sugar.
- Physical Inactivity: Lack of regular exercise.
- Tobacco Use: Smoking and exposure to secondhand smoke.
- Harmful Use of Alcohol: Excessive alcohol consumption.
Intermediate Risk Factors
These risk factors often manifest as clinical measurements:
- Raised Blood Pressure (Hypertension)
- Raised Blood Glucose (Diabetes)
- Raised Blood Lipids (Cholesterol)
- Overweight and Obesity
heart failure symptoms
heart disease symptoms
congenital heart disease
heart problems symptoms
heart problems
symptoms of heart blockage in females
cardiovascular
ischemic heart disease
cardiovascular disease symptoms
Underlying Determinants
Several broader social, economic, and environmental factors contribute to the prevalence of CVDs:
- Globalization and Urbanization: Changes in lifestyle and diet patterns.
- Population Aging: Increased risk with age.
- Poverty and Stress: Socioeconomic challenges.
- Hereditary Factors: Genetic predisposition to cardiovascular conditions.
Preventive Measures
Effective prevention strategies involve addressing both behavioral and intermediate risk factors through lifestyle modifications and medical interventions.
Lifestyle Modifications
- Healthy Diet: Increase intake of fruits, vegetables, whole grains, and lean proteins while reducing salt, sugar, and unhealthy fats.
- Regular Physical Activity: Engage in at least 150 minutes of moderate-intensity exercise per week.
- Cessation of Tobacco Use: Quit smoking and avoid secondhand smoke.
- Moderate Alcohol Consumption: Limit alcohol intake according to health guidelines.
Health Policies
Implementing health policies that create supportive environments for healthy choices is crucial. This includes:
- Reducing the availability of unhealthy food options.
- Promoting physical activity through urban planning.
- Implementing tobacco control measures.
- Ensuring access to healthcare services for early detection and treatment.
Management of Cardiovascular Diseases
Medical Interventions
Patients with cardiovascular diseases should have access to appropriate medical care, including medications and surgeries when necessary.
Common Medications
- Aspirin: To prevent blood clots.
- Beta-blockers: To manage heart rate and blood pressure.
- Angiotensin-Converting Enzyme (ACE) Inhibitors: To lower blood pressure and protect the heart.
- Statins: To reduce cholesterol levels.
Surgical Treatments
- Coronary Artery Bypass Surgery
- Balloon Angioplasty: To open blocked arteries.
- Valve Repair and Replacement
- Heart Transplantation
- Artificial Heart Operations
Medical Devices
- Pacemakers: To regulate heartbeats.
- Prosthetic Valves: To replace damaged valves.
- Patches: For closing holes in the heart.
Reducing the Burden of Cardiovascular Diseases
Health System Strengthening
Incorporating cardiovascular disease management into universal health coverage packages is essential. Significant investments and reorientations of health systems are needed to manage CVDs effectively.
Cost-Effective Interventions
Evidence shows that hypertension programs can be efficiently implemented at the primary care level, reducing the incidence of coronary heart disease and stroke.
Global Initiatives
WHO’s “Global Action Plan for the Prevention and Control of NCDs 2013-2020” aims to reduce premature deaths from non-communicable diseases by
25% by 2025 through various targets, including those specifically focused on cardiovascular diseases:
- Target 6: Reduce the global prevalence of raised blood pressure by 25%.
- Target 8: Ensure that at least 50% of eligible people receive drug therapy and counseling to prevent heart attacks and strokes.
- Target 9: Achieve 80% availability of essential medicines and technologies to treat major non-communicable diseases.
Conclusion
Cardiovascular diseases are a significant global health challenge, but with comprehensive understanding, prevention, and management strategies, their burden can be significantly reduced. By adopting healthier lifestyles, improving health policies, and ensuring access to effective medical care, we can work towards reducing the incidence and impact of CVDs.



